There is a clear link between the presence of oral bacteria and systemic diseases in different parts of the body. Some of the most well-known of those “systemic” links, of course, are the connections between oral health and serious conditions like diabetes, heart disease, and several different cancers of the body including mouth and throat cancers.
Keep reading to learn more about the deeper relationship between the health of the oral cavity and various health conditions, the impact this health link has on those suffering from these conditions, and how today’s dental professionals are engaging in proactive management of common diseases with practical, effective dental treatment plans.
The Oral-Systemic Relationship
In 2000, the Surgeon General issued a report on the status of oral health in the US, recognizing an association between periodontal diseases and cardiovascular health, stroke, diabetes, and adverse pregnancy outcomes, calling for more research to determine whether causation may be established.
The Surgeon General’s report of 2000 was updated in 2021, echoing the original statement while stressing the social and behavioral inequities that limit access to care. The report1 provides a call to action, urging policymakers, healthcare professionals, and the community to “work together to provide integrated oral, medical, and behavioral health care” while addressing “social, economic, or other systemic inequities that affect oral health behaviors and access to care.” What is at the core of the oral systemic relationship?
Inflammation in the Oral Cavity
When it comes to oral health today, there’s an abundance of evidence indicating that chronic inflammation in the oral cavity can directly, and significantly, affect immune response. For example, many inflammatory and autoimmune diseases have been shown to develop in the oral mucosa, such as periodontitis, Sjögren’s syndrome, and OLP.
Periodontitis in particular is initiated by the accumulation of bacterial plaque, subsequent tissue damage, and bone loss due to host immune responses and inappropriate inflammation. The oral cavity, when poorly maintained, serves as a reservoir of pathogenic bacteria that quickly enter the bloodstream and affect distant-site or systemic pathologies (systemic endotoxemia or bacteremia).
What are some of the most common conditions that are thought to be linked to the oral cavity and how does this “systemic link” work?
Oral Health and Heart Disease
Patients with chronic gum conditions such as gingivitis or advanced periodontal disease have a higher risk for heart disease caused by poor oral health, particularly if it remains undiagnosed and unmanaged. The bacteria that infect the gums and cause gingivitis and periodontitis also travel to blood vessels elsewhere in the body where they cause blood vessel inflammation and damage; tiny blood clots, heart attack, and stroke may follow.
Anxiety, Depression, and Mental Health
Mental health affects the entirety of the human body, including its oral health. Patients with anxiety and depression may engage in behaviors that lead to poor nutrition (consuming sugary foods or beverages), low energy, and tobacco, alcohol, or drug use. Those who face mental health challenges are more prone to oral health conditions including periodontitis and other teeth and gum problems.
Diabetes and Oral Health
People with diabetes have a higher chance of having periodontal (gum) disease, an infection of the gum and bone that hold the teeth in place. Periodontal disease can lead to pain, bad breath that doesn’t go away, chewing difficulties, and even tooth loss (edentulism). 1 in 5 cases of total tooth loss, in fact, is linked to diabetes. Diabetes raises glucose levels in the mouth, and numerous dental problems can arise as a result, as those added sugars promote bacteria growth, infection, and bad breath (halitosis). The long-term oral complications resulting from unmanaged diabetes are significant.
Oral Health and Cancer
More than one-third of all cancer patients develop complications that affect the mouth, according to the National Institute of Dental and Craniofacial Research. Cancer and some treatments including chemotherapy can weaken the body’s immune system. Poor oral health prior to cancer treatments may lead to infection and ultimately result in delays in a patient’s cancer treatment. Even with good oral health, many cancer treatments affect a person’s mouth, teeth, and salivary glands, making it difficult for patients to eat, talk, chew or swallow.
Oral Health and Pregnancy
Pregnancy may make women more prone to periodontal (gum) disease and cavities. Oral health may be considered an important part of prenatal care, given that poor oral health during pregnancy can lead to poor health outcomes for the mother and baby. Nearly 60 to 75% of pregnant women have gingivitis3, an early stage of periodontal disease that occurs when the gums become red and swollen from inflammation that may be aggravated by changing hormones during pregnancy.
Alzheimer’s Disease and Oral Health
There is increasing evidence that those suffering from progressive neurodegenerative conditions like Alzheimer’s disease and dementia have an increased likelihood of oral hygiene issues. One recent study, in fact, suggested that the same bacteria responsible for gingivitis may also be connected to diseases like Alzheimer’s. While an estimated4 50 million are expected to experience the effects of the disease by 2050, research continues to suggest5 that good oral hygiene can play a role in limiting the impact of the condition.
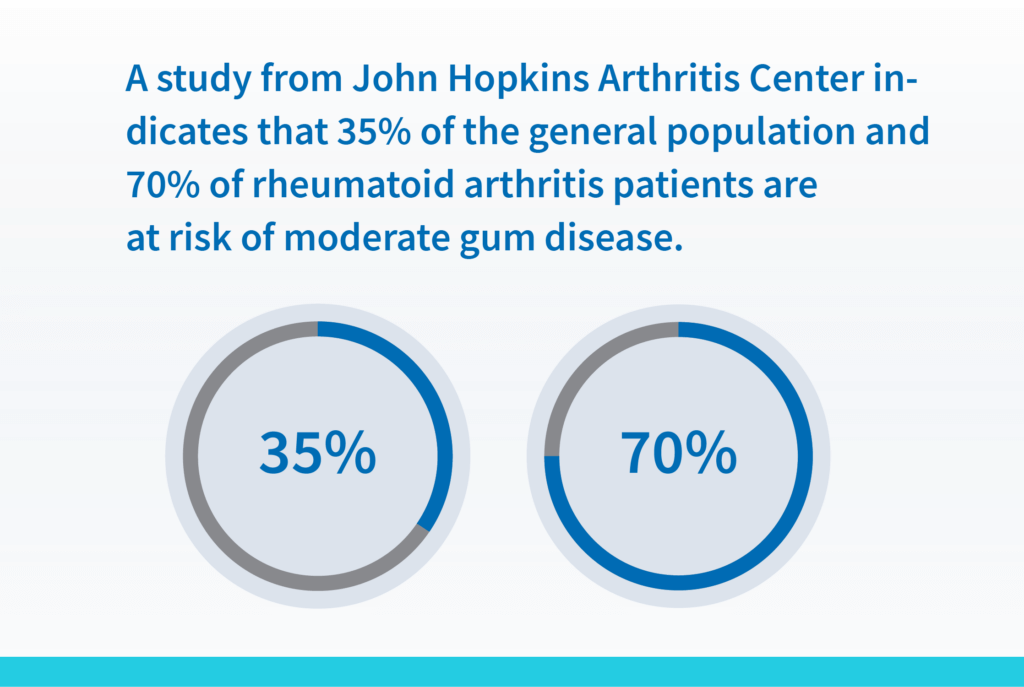
Oral Health and Rheumatoid Arthritis
Chronic inflammatory diseases such as rheumatoid arthritis are proving to have a clear and direct connection to oral health. A study from John Hopkins Arthritis Center, for example, indicated that 70% of RA patients surveyed had at least moderate gum disease, compared to 35% of the general population. Those suffering from rheumatoid arthritis can also develop other serious oral health conditions including Sjögren’s syndrome, a condition that causes inflammation in the salivary glands.
Let’s Work Together to Provide Integrated Oral, Medical, and Behavioral Health Care
MouthWatch is a leader in innovative teledentistry solutions, digital case presentation tools, and intraoral imaging devices.
TeleDent, the complete teledentistry platform byMouthWatch, LLC was built from the ground up for dental professionals and their patients. Features such as an intuitive, mobile-friendly patient portal, text messaging, and online patient intake, make it easier to connect with patients in the safe and convenient way they now expect. New patient consults, post-op evaluations, home care instructions, specialist referrals and emergency triage can all be conducted with the highest degree of simplicity, security, and safety.
Dedicated to continually finding new ways to improve the dental health experience for both patient and provider, contact our team today to learn how you can work with MouthWatch to provide a better integrated oral, medical and behavioral health care experience.
1National Institutes of Health. Oral Health Care in America: Advances and Challenges. Bethesda, MD: US Department of Health and Human Services, National Institutes of Health, National Institute of Dental and Craniofacial Research; 2021.
2Corbella S, Taschieri S, Del Fabbro M, Francetti L, Weinstein R, Ferrazzi E. Adverse pregnancy outcomes and periodontitis: A systematic review and meta-analysis exploring potential association. Quintessence Int. 2016 Mar;47(3):193-204. doi: 10.3290/j.qi.a34980.
3American Dental Association Council on Access, Prevention, and Interprofessional Relations, 2006.
4ALZ.org: Alzheimer’s Facts & Figures
5Good oral health may protect against Alzheimers
6Holmer J, Eriksdotter M, Schultzberg M, Pussinen PJ, Buhlin K. Association between periodontitis and risk of Alzheimer’s disease, mild cognitive impairment and subjective cognitive decline: A case-control study. J Clin Periodontol. 2018;45:1287–98. PubMed

![Several epidemiological studies of the association between oral health and CVD indicate that people with periodontal disease are at increased risk up to 25% for CVD [CITATION] and 84.4% of individuals with CVD had periodontal disease compared to only 22.5% in individuals without CVD.](https://www.mouthwatch.com/wp-content/uploads/MouthWatch_Landing_Page_Graphic_4-1024x687.png)